Neuromotor Research Clinic
NEUROMOTOR RESEARCH CLINIC
About the Neuromotor Research Clinic
Located in Roanoke, Virginia, the Fralin Biomedical Research Institute Neuromotor Research Clinic is where Virginia Tech scientists create new treatment strategies for children and young adults with cerebral palsy and other neuromotor movement disorders.
For many years, cerebral palsy was considered a static condition with only limited opportunities to teach children to use their impaired arms or legs. Research supported by the National Institutes of Health (NIH) over the past several decades has led to a new understanding of the brain’s capacity for functional reorganization through focused, intensive training that taps into neuroplasticity processes intrinsic to the nerve cells of the brain throughout life, even after brain disease or injury.
The directors of the Fralin Biomedical Research Institute's Neuromotor Research Clinic, Dr. Sharon Ramey and Dr. Stephanie DeLuca, pioneered the use of a high-intensity therapeutic intervention that has allowed children with weakness on one side of their bodies — a hallmark of one form of cerebral palsy known as hemiparesis — to make large, rapid, and enduring gains in their everyday neuromotor skills.
The Fralin Biomedical Research Institute Neuromotor Research Clinic seeks to enable children with neuromotor impairment to make large, rapid, and enduring gains in their everyday neuromotor skills. To improve the children’s abilities, our therapists use a set of rehabilitation approaches based on intensive therapeutic dosages guided by learning principles. Broadly, we call these approaches ACQUIRE therapy. ACQUIRE therapy involves a systematic shaping of brain function and motor behavior through a cycle of movement, reinforcement, repetition, and refinement. The children work diligently to make steady improvements while engaged in fun activities, games, and self-help skills. The children also help set their own goals and the therapists provide multiple supports to allow each child to realize major gains.
To ensure long-term effectiveness, our therapists work in a homelike or community setting so new skills become part of a child’s everyday routine. The therapists educate parents about ACQUIRE and develop a transition plan that engages the entire family. We measure each child’s progress using standardized assessments to ensure we monitor progress closely.
For children with hemiparesis or asymmetry between the abilities of the two sides of their body, your child’s intensive burst of treatment may involve constraint of your child’s arm and hand on the side that has more mobility (your child’s more functional arm and hand). The constraint used will be a lightweight cast, specially fitted for your child. The casting procedure is designed to immobilize the functional arm and hand to help facilitate use of the involved arm and hand. This intensive treatment is based on previous research surrounding Pediatric Constraint-Induced Movement Therapy (P-CIMT). The ACQUIRE Therapy model began with this form of treatment. While it now extends beyond this single form of therapy, the guidelines (beyond the constraint) were originally developed in clinical trials to inform this treatment approach.
Children are eligible for treatment when the following criteria are met:
(1) demonstrated significant motor impairment attributable neurological condition that presents with asymmetry between the two sides of the body;
(2) between 2 and 21 years old; and
(3) does not have any serious complicating conditions or acute medical concerns (seizures must be under control).
For children with hemiparesis or asymmetry between the abilities of the two sides of their body your child’s intensive burst of treatment may involve constraint of your child’s arm and hand on the side that has more mobility (your child’s more functional arm and hand). The constraint used will be a lightweight cast, specially fitted for your child. The casting procedure is designed to immobilize the functional arm and hand in order to help facilitate use of the involved arm and hand. This intensive treatment is based on previous research surrounding Pediatric Constraint-Induced Movement Therapy (P-CIMT). The ACQUIRE Therapy model began with this form of treatment. While it now extends beyond this single form of therapy, the guidelines (beyond the constraint) were originally developed in clinical trials to inform this treatment approach.
Children are eligible for treatment when the following criteria are met:
(1) significant motor impairment attributable neurological condition that presents with asymmetry between the two sides of the body;
(2) between 8 and 36 months old; and
(3) does not have any serious complicating conditions or acute medical concerns (seizures must be under control).
This protocol is aimed at helping children who have more global levels of motor impairment gain increased motor function. Successive approximation for motor skills and intensive therapeutic bursts are guiding principles.
Children are eligible for treatment when they meet the following criteria:
(1) significant motor impairment attributable neurological condition, which presents with motor impairments that may involve all four extremities;
(2) between 12 months and 21 years old; and
(3) no serious complicating conditions or acute medical concerns (seizures must be under control).
Similar, to the above we have now worked with a variety of children with diagnoses who have delays in development that often include areas beyond just motor skills. It is important to note that we have primarily focused on diagnoses that do manifest in some manner with motor delays of limitations, but we have now successfully used our learning protocols and intensive therapeutic bursts to target other domains of development (e.g., communication, appropriate social skills (reciprocal play), and processing to follow multiple step requests/activities.
Children are eligible for treatment when they meet the following criteria:
(1) significant impairments or delays in multiple areas or development attributable neurological condition that presents with some motor challenges;
(2) between 12 months and 21 years old; and
(3) no serious complicating conditions or acute medical concerns (seizures must be under control).
The National Pediatric Rehabilitation Resource Center, also known as C-PROGRESS, helps clinical scientists studying pediatric rehabilitation by funding pilot studies, providing mentorship, and offering training and tools to support clinical trials research. C-PROGRESS stands for the Center for Pediatric Rehabilitation: Growing Research, Education, and Sharing Science, the center’s primary objective is to “see progress” in the emerging field of pediatric rehabilitation science. The Center is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Neurological Disorders and Stroke, and the National Institute of Biomedical Imaging and Bioengineering. C-PROGRESS is one of six national centers in the Medical Rehabilitation Resource Network (MR3).
Support Our Research
Your donation to the Neuromotor Research Clinic will help:
- It costs $24,000 annually to deliver therapy to a child
- Support research into new treatment strategies for children and young adults
- Offset the cost of housing and related expenses for families
- Train health professionals and caregivers in intensive therapy techniques to help children lead fuller lives.
FRIENDS OF ACQUIRE
Our team has been honored to care for all of the children and families who have come to the Fralin Biomedical Research Institute at VTC Neuromotor Research Clinic. We want to introduce you to Friends of ACQUIRE, a group for parents, relatives, and friends who want to learn more about our research and discoveries in pediatric rehabilitation.
NEUROMOTOR RESEARCH CLINIC VIDEO NEWS
-
Home Item
 DeLuca Lab , home
DeLuca Lab , homeThe DeLuca lab has examined the impact of intensive neurorehabilitation treatments on children and adults with neuromotor impairments for more than 25 years.
-
Home Item
 C. Ramey Lab , home
C. Ramey Lab , homeThe Ramey Lab's program of research centers on the role of experience – across the human lifespan - in the development of competence and robust health.
-
Home Item
 S.L. Ramey Lab , home
S.L. Ramey Lab , homeThe Landesman Ramey Lab addresses the contribution of early experience from before conception to later health and development and the development and testing of highly promising treatments for children with disabilities and at-risk conditions.
-
Article Item
-
Article Item
-
Article Item
-
Article ItemIt’s the ‘thing in my life that shaped me the most,’ participant says of life-changing therapy , article
After experiencing a stroke in utero that caused weakness on the left side of her body, Keya Shapiro found a home at the Fralin Biomedical Research Institute’s Neuromotor Research Clinic, which is celebrating 10 years of research into the therapy.
Date: Jan 17, 2024 - -
Article ItemMoving forward: Neuroscientist explores movement, rehabilitation in public lecture , article
Motor learning expert and National Academy of Sciences member Amy Bastian will deliver the next Maury Strauss Distinguished Public Lecture on Nov. 2 at the Fralin Biomedical Research Institute.
Date: Oct 27, 2023 - -
Article ItemFralin Biomedical Research Institute at VTC: Growth of an innovator , article
Since its founding in 2010, the research institute has become a focal point for biomedical research across Virginia Tech. It now has more than 450 faculty, staff, and students in Roanoke and Washington, D.C., supporting research fueled by $173.7 million in external grants.
Date: Aug 29, 2023 - -
Article ItemTherapy framework reveals promise for intensive pediatric rehabilitation for children with motor disabilities , article
Virginia Tech researchers with the Fralin Biomedical Research Institute at VTC have demonstrated that children with a wide range of diagnoses that affect their motor function improve after receiving intensive pediatric rehabilitation called ACQUIRE Therapy.
Date: Jun 16, 2023 - -
Article Item‘The right place’: Sisters with rare disorder find help , article
Sisters with a very rare genetic mutation that affects brain development are benefitting from a form of intensive therapy being studied at the Fralin Biomedical Research Institute Neuromotor Research Clinic.
Date: Feb 03, 2023 - -
Article ItemFralin Biomedical Research Institute occupational therapists train colleagues, treat children in Morocco clinic , article
Kelsey Burke and Megan Price, occupational therapists in the Neuromotor Research Clinic at the Fralin Biomedical Research Institute at VTC, took a personal volunteer trip to Morocco with a humanitarian group last year. They educated therapists and parents in pediatric therapy techniques.
Date: Mar 02, 2022 - -
Article ItemRare disease research gives families hope, ‘vital’ to advancing medicine , article
Rare diseases afflict 300 million people worldwide. Fralin Biomedical Research Institute at VTC researchers are bridging a gap in scientific knowledge by studying some of the diseases that together add up to a formidable public health challenge. Feb. 28 marks the 14th international Rare Disease Day.
Date: Feb 28, 2022 - -
Article ItemLarge doses of intensive therapy better for children with cerebral palsy, Virginia Tech scientists, partners find , article
The study, funded by the National Institutes of Health’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, shows that higher doses of Constraint-Induced Movement Therapy – 20 three-hour sessions over four weeks – yield significant and lasting improvement in use of their arms and hands, especially in everyday functional activities.
Date: Oct 14, 2021 - -
Article ItemScientists say active early learning shapes the adult brain , article
Through the Abecedarian Project, an early education, randomized controlled trial that has followed children since 1971, Virginia Tech researchers, including Craig Ramey, Sharon Landesman Ramey, and Read Montague, revealed new discoveries about brain structure that have continued through decades.
Date: May 31, 2021 - -
Article ItemFralin Biomedical Research Institute graduate student awarded NIH Fellowship to examine balance, walking in children with cerebral palsy , article
Hassan Farah, a Virginia Tech translational biology, medicine, and health graduate student, has been awarded a $98,000 National Institutes of Health grant that will fund his remaining predoctoral research. Farah is studying the limb biomechanics, joint movements, and loading in children with cerebral palsy.
Date: Feb 01, 2021 - -
Article ItemFralin Biomedical Research Institute, partners pioneer nation’s first pediatric rehabilitation resource center , article
Research partners across three institutions are opening the nation’s first and only resource center, known as C-PROGRESS, dedicated to promoting clinical trials research in the rapidly expanding field of pediatric rehabilitation.
Date: Jul 21, 2020 - -
Article ItemVirginia Tech faculty receive top honors from the American Association for the Advancement of Science , article
Elected by their peers and representing a broad range of AAAS “sections,” including statistics, neuroscience, engineering, psychology, and geology/geography, the Virginia Tech professors are among 443 newly elected scholars.
Date: Nov 26, 2019 - -
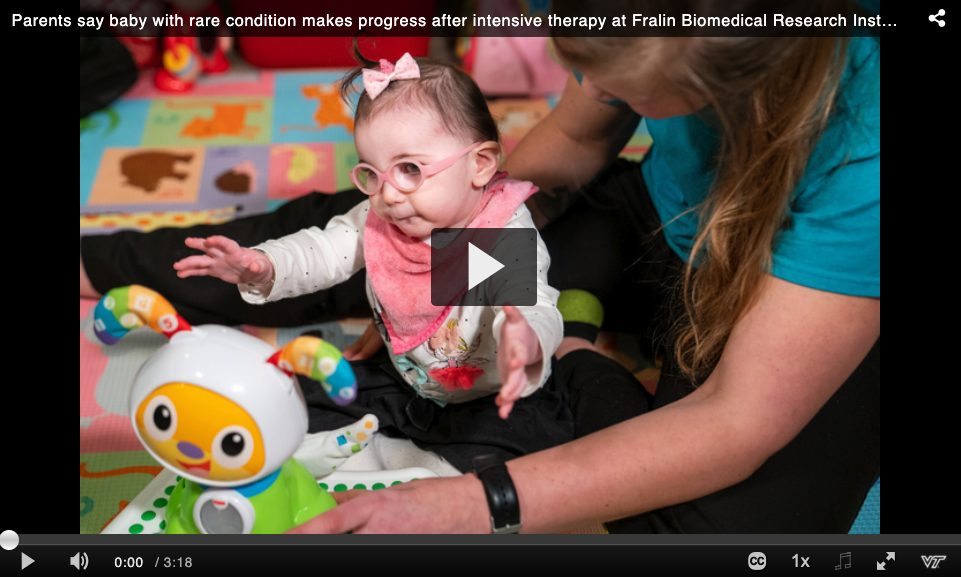
Article ItemNation’s first clinical trial for rehabilitating infant stroke victims to begin , article
Called I-ACQUIRE, the Phase III clinic trial will examine the effectiveness of a pediatric therapy to increase upper extremity skills, gross motor development, and cognition in 240 children nationwide who experienced strokes when they were under 4 weeks old.
Date: Mar 25, 2019 - -
Article ItemVTC School of Medicine names Fralin Biomedical Research Institute’s Stephanie DeLuca as 2019 Outstanding Research Mentor , article
DeLuca, a developmental psychologist who also holds faculty appointments in the VTCSOM and the Virginia Tech College of Science, has been a Fralin Biomedical Research Institute faculty member for six years. She develops neurorehabilitation treatment techniques for both children and adults.
Date: Mar 05, 2019 - -
Article ItemVTCRI researcher, VTCSOM student team up to teach innovative treatment to Vietnamese therapists , article
The therapy is based on studies of the effects of prolonged disuse by parts of the brain that may occur as a result of cerebral palsy or after stroke.
Date: Jun 06, 2018 - -
Article ItemVTCRI researchers join forces to improve life for children with genetic disorder , article
The accomplishments of three girls who received intensive therapy based on innovative pediatric neurorehabilitation research at the VTCRI have been documented in a report published in BMC Research Notes.
Date: Mar 22, 2018 -
NEUROMOTOR RESEARCH CLINIC
MEDIA COVERAGE
-
Redirect ItemSmith College: Going Back — To Give Back , redirect Date: Sep 10, 2025 -
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect ItemScience Daily: Child-centric approach: Blueprint to improve communities , redirect Date: Dec 01, 2023 -
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect ItemWSLS: Local researchers leading study on infant stroke rehabilitation , redirect Date: Mar 26, 2019 -
-
Redirect Item
-
Redirect Item
-
Redirect Item
-
Redirect ItemThe Roanoke Times: VTCRI research gives family hope , redirect Date: Feb 13, 2017 -
-
Redirect Item
-
Redirect Item
-
Redirect ItemSan Francisco Chronicle: Va research institute to study cerebral palsy , redirect Date: Aug 16, 2013 -
-
Redirect Item
-
Redirect ItemWVTF: New research clinic studies children with cerebral palsy , redirect Date: Aug 15, 2013 -
-
Redirect ItemWSLS: New Neuromotor Research Clinic at VTC , redirect Date: Aug 15, 2013 -
-
Redirect Item
-
Redirect ItemPsychreg: Scientists Say Active Early Learning Shapes the Adult Brain , redirect Date: Jun 05, 2021 -